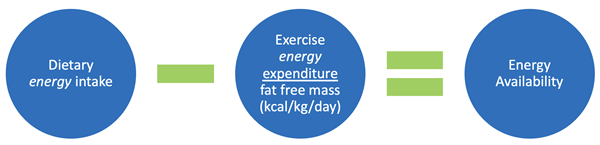
Energy availability is described using a spectrum:
- Optimal energy availability
- Reduced energy availability
- Unintentional: inadequate dietary intake and/or excessive exercise
- Intentional: disordered eating behaviors
- Low energy availability
- Eating Disorder: clinical mental disorder defined by DSM-V
- Disordered Eating: various abnormal eating behaviors including restrictive eating, fasting, frequently skipped meals, diet pills, laxatives, diuretics, enemas, overeating and binging and purging
How much dietary intake is normal?
Optimal energy availability is 45 kcal/kg fat free mass per day. This is known to support physically active women. Anything less than 30 kcal/kg fat free mass per day contributes to negative metabolic, reproductive and bone health related changes are seen below this level.
- An athlete’s weight should be >90% of expected body weight.
- Low BMI is a strong predictor of low bone mineral density and stress fractures.
What are normal and abnormal menstrual cycles?
Also called eumenorrhea, the typical cycle occurs every 28 days and lasts about 7 days. In cases where the cycle occurs less frequently, specifically more than 35 days apart, it is called oligomenorrhea. The absence of the cycle, amenorrhea, may be primary or secondary. In cases of low energy availability, the absence is further defined as functional hypothalamic amenorrhea.
How are estrogen and progesterone associated with musculoskeletal health?
Beyond the reproductive cycle, these hormones are also important in bone health.
- Stimulates osteoblasts
- Inhibits osteoclasts
- Muscle activation
- Ligament and tendon stiffness
- Suppresses hormones that cause articular cartilage breakdown
What is peak bone mass and what can positively influence it in female athletes?
Peak bone mass is a measure of bone mineral density that is used to assess bone health and risk for injury such as fracture, stress fracture and osteoporosis later in life. Ninety percent of peak bone mass is obtained by age 18 in females and age 20 in males. In young adults, bone mineral density 10% higher than the mean may reduce risk of fractures as well as delay the onset osteoporosis as much as 13 years. Therefore, attention to bone mass during childhood and adolescence is of utmost importance.
Genetics is the main determinant of peak bone mass. The following items also impact peak bone mass:
- Mechanical forces
- Gender
- Hormones
- Nutrition
- Physical activity or other outside risk factors.
Early puberty is the most crucial time to positively influence peak bone mass with weightbearing sports and high-impact exercises. Studies have found that participation in sports can increase bone mass by as much as 10%.
What problems occur from low energy availability?
Several systems are affected, and the consequences compound in a cascade. Here are some key messages to keep in mind.
Bone Health
- A reduction in bone formation caused by suppression in hormones is possible.
- Low bone mineral density is known to increase the risk of stress fractures.
- Changes from low bone mineral density may be irreversible.
- DXA scans are recommended based on the presence of specific high and or moderate risk factors.
Reproductive System
- Functional hypothalamic amenorrhea is a diagnosis of exclusion.
- Other causes of abnormal menstrual cycles should be considered.
- Young athletes believe it is a normal response to training, but it is not.
Tip for young athletes: encourage females to be prepared for their period with supplies (feminine hygiene products, clean clothes, plastic bag) and to monitor their menstrual cycle to adjust training as needed.
Cardiovascular Health
Studies have shown that history of prolonged irregular menstrual cycles may negatively affect cardiovascular health and has shown possible association with:
- Coronary artery disease
- Endothelial dysfunction
- Unfavorable lipid profiles and increased LDL
- Triad may reduce performance and training responses, delay or extend healing and cause fatigue.
What is Relative Energy Deficiency in Sports?
Also referred to as RED-S, this is an evolution of the concept recognizing impaired physiological functioning caused by relative energy deficiency. This includes but is not limited to impairments of metabolic rate, menstrual function, bone health, immunity, protein synthesis and cardiovascular health.
How is male athlete triad different than female athlete triad?
Reproductive suppression is seen in males in these forms:
- Low testosterone (T)
- Oligospermia
- Decreased libido
When is screening for triad or RED-S most appropriate?
Well visits such as during a pre-participation physical evaluation (PPE) or the yearly check-up and any time an athlete presents for a recurrent injury, bone stress injury or other illness. To diagnose the condition, only one of the three components must be present. Evaluate further with any positive finding.
What are appropriate screening questions?
The Female and Male Athlete Triad Coalition provides a list of 15 screening questions. These are consistent with the American Academy of Pediatrics 2019 Preparticipation Physical Evaluation recommendations and can help to guide further discussion and assessment.
- Do you worry about your weight or body composition?
- Do you limit or carefully control the foods that you eat?
- Do you try to lose weight to meet weight or image/appearance requirements in your sport?
- Does your weight affect the way you feel about yourself?
- Do you worry that you have lost control over how much you eat?
- Do you cause yourself to vomit or use diuretics or laxatives after you eat?
- Do you currently or have you ever suffered from an eating disorder?
- Do you ever eat in secret?
- What age was your first menstrual period?
- Do you have monthly menstrual cycles?
- How many menstrual cycles have you had in the last year?
- Have you ever had a stress fracture?
What are other risk factors of RED-S?
- History of menstrual irregularities
- History of stress fractures, family history of osteoporosis
- Depression
- Perfectionistic or obsessive personalities
- Overtraining
- Non-healing injuries
- Inappropriate coaching
- Early sports specialization
What are the treatment and recovery expectations for athletes with female athlete triad?
The primary goal is restoration and normalization of body weight, to restore menses and to improve bone health. Rest or modified training may be recommended depending on the risk of injury or presence of concerning symptoms. A collaborative treatment approach includes a physician with experience treating athletes with triad, a dietitian, a psychologist and sometimes other specialists. Treatment with a birth control pill may lead to the false belief that the natural process has been restored, however, these do not cause the return of normal menses.
Returning to sports should be considered using a cumulative risk assessment. Recovery occurs first with energy status, then menstrual status and then bone health. Earlier diagnosis reduces the length of recovery and hopefully prevents irreversible changes. Resumption of normal menses can sometimes take months or longer, reversal of low bone mineral density can sometimes take year or longer, and sometimes may be irreversible.
What are strategies to optimize bone health in young athletes?
- Focus on risk factors to address biological risk factors for low bone mineral density
- Ensure adequate calcium and vitamin D, nutrition and overall energy availability
- Encourage adequate sleep as it may promote bone health
- Appropriate loading activities during the “critical period” of youth (early puberty)
About the Speaker
Jane S. Chung, M.D., is a pediatric sports medicine physician at Scottish Rite for Children Orthopedics and Sports Medicine Center in Frisco, Texas. She is passionate about the health and safety of young athletes and cares for pediatric sport-related medical and musculoskeletal conditions. Chung loves to teach other provider, parents and athletes about the unique needs of female athletes during crucial growing years.