Return to Weight Lifting: A Guide for Young Athletes After Injury
Patients in the Scottish Rite for Children sports medicine clinic may lift weights as part of their primary sport training or with a strength and conditioning coach to supplement sport-specific training. When an injured athlete is released back to activities that include weight lifting, Scottish Rite for Children athletic trainer Allen Tutton, M.S., L.A.T., A.T.C., C.E.S., provides systematic instructions to ensure a safe, progressive return to training. Tutton is uniquely qualified with skills as both an athletic trainer and a corrective exercise specialist (CES). A certification from the National Academy of Sports Medicine, the C.E.S., requires a solid understanding of the interrelationship of movement quality and exercise, a must for strength and conditioning advice for young athletes. Here are his tips for safe weight lifting:
Before You Start
- Focus on form and technique instead of the amount of weight or number of repetitions.
- Increase your working weight slowly after an injury or a long break from training.
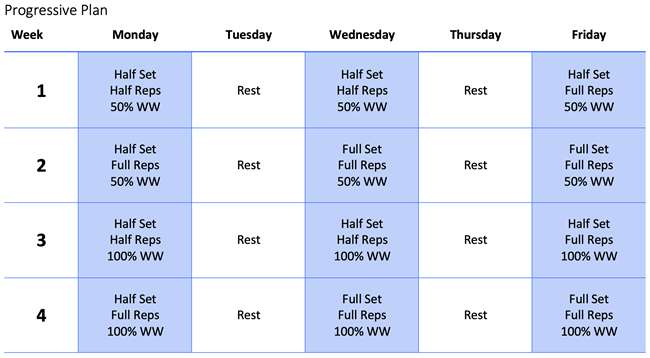
- Working weight (WW) is the repetition (not max) weight used in your workout on a normal day.
Warm-up and Lifting
- A warm-up is necessary to help you perform your workout at your best.
- An optimal, dynamic warm-up includes upper and lower body stretches as well as light jogging.
- Have a spotter with you when you begin lifting.
- If you feel any abnormal discomfort, you must stop and rest 48 hours before trying the step again.
- If your working weight is too heavy, decrease the weight used.
Terms to Know
- Repetitions (reps) = number of times you perform the exercise before a rest.
- Set = number of times you repeat the exercise and rest.
Wrap It Up
- Each workout should not last longer than one hour.
- Stay hydrated and rest at least 24 hours between sessions.
Managing Load: Preventing Overuse Injuries
Load can be measured in several ways:
- Total work or repetitions done in a day.
- Total weight lifted in a day.
- Collection of work throughout a period, such as a week or a month.
Rushi Patel, P.T., D.P.T., SCCE, says, “A combination of how much weight is lifted, how often and for how long can all play a role in potential overuse injuries in the weight room.”
Patel offers these tips to minimize the risk of injuries:
- All sport-related training should be considered part of the overall load. Times to reduce the weight or intensity of a weight-lifting routine include:
- Starting a new sport or returning to sport after a break.
- Preseason sport-specific intense training.
- Focused sport-specific training in a camp or when learning a new skill.
- Monitor how you feel in the first 24-48 hours after a workout. Excessive joint pain or soreness that lingers might be a sign to modify some activities related to your workouts.
To learn how nutrition can play a role in safe and effective strength training programs, read this article.