Sports Medicine Year in Review
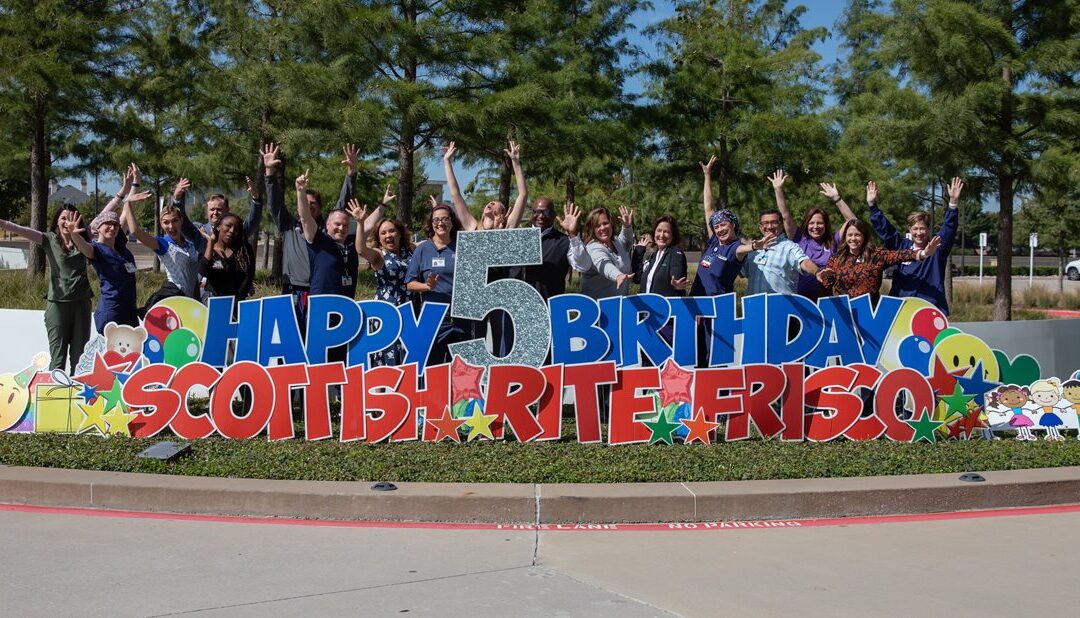
Scottish Rite for Children Orthopedic and Sports Medicine Center has had an exciting year! We celebrated our fifth birthday in the beautiful facility where we serve children with a variety of pediatric orthopedic needs requiring all levels of care from observation to complex reconstructive surgery. Our mission is often described having three elements, clinical care, teaching and research. Together, they provide a rich experience for patients and trainees and help to define pediatric orthopedics across the world.
Here are a few updates from the Sports Medicine team.
CLINICAL CARE
In the sports medicine clinic, we see more than 16,000 visits each year, and that number continues to grow. Recognized again for excellence in patient experience, our team focuses on educating the patients and families and providing outstanding care so that patients have the outcome they desire. Our work to integrate screening for psychological and nutritional needs help our patients succeed in their rehabilitation and return to sport efforts.
TEACHING
Pediatric sports medicine is a relatively new subspecialty in pediatric orthopedics. In fact, only a handful of organizations have an ACGME-accredited* fellowship program focused on this area. We are very excited to share that we are currently in the process of selecting our first fellow to join our team in 2024. This year-long training program offers a sports medicine surgeon the opportunity to train alongside our experts in the clinic, on the sidelines and in the operating room. In the past year, we had 13 orthopedic residents rotate through our clinic to learn about care and research in pediatric sports medicine.
RESEARCH
This year, our team published more than 20 articles in prestigious medical journals. Many authored by our medical staff and trainees and others were collaboration with peers in the Pediatric Research in Sports Medicine (PRiSM) Society. Here are findings that are being presented at national and international conferences and have the potential to change sports medicine in the areas of diagnostics, clinical care, return-to-sport decision making and injury prevention.
- In a study of 2000 pediatric and adolescent surgical meniscus repairs, complications occurred in approximately one of every 10. This study has continued, and it appears the rate may actually be lower. This information helps surgeons discuss risks and benefits of surgery and provides a baseline for improvements in care.
- Kneecap (patellar) instability most commonly affects skeletally immature pediatric patients with open growth plates. Scottish Rite’s work has shown that medial patellofemoral ligament reconstruction should be the primary treatment for first-time patellar instability in skeletally immature patients.
- In a survey of 244 parents, mostly reporting soccer as their child’s primary sport, one in five reported they were not aware that injury prevention programs for ACL injuries are available although studies show these programs have high rates of success. This information helps the authors formulate specific education and outreach plans. Learn more about ACL prevention programs.
- An evaluation of sleep quality in 177 soccer players found that those who have had a concussion reported sleep quality deficits more often than those with no history of a concussion. This information suggests that athletes who sustain concussions may need interventions to improve sleep quality. This is consistent with earlier findings.
- Middle school athletes were evaluated using a standard assessment of gross motor skills, and it was found that none of them achieved a mastery score. This information is alarming in the age where one in three specialize in a sport at a young age but haven’t mastered basic movement skills, which puts them at an increased risk of injury.
- In responses to 500 presurgical nutrition screening questionnaires, developed by Scottish Rite certified sports dietitian and other staff, the review found that one in three athletes regularly skip one meal a day. This information suggests we should continue to educate young athletes on proper fueling for health, growth and sports.
The Sports Medicine team is presenting results from more than 25 projects at a national meeting for the PRiSM Society in January. This work is made possible by our patients, national grants, generous donors and many student trainees learning about pediatric orthopedics and sports medicine.
Learn how healthy athletes can volunteer for a study or you can donate.
* The Accreditation Council for Graduate Medical Education (ACGME) is the accrediting body for graduate medical education. They hold programs to standards that prepare physicians in nearly 200 specialties.











