A Shared Passion to Protect and Serve
Published in Rite Up, 2023 – Issue 3.
Last summer, the Inpatient Unit at Scottish Rite for Children had extra security and cuteness overload in the form of a 4-year-old patient lovingly referred to as Policeman Joseph. Donning a police vest, badge, walkie-talkie and binoculars, Joseph, of Gonzales, Louisiana, made daily rounds to keep his fellow patients safe. “He’s got a huge personality stuffed inside a little body,” says Randi, his mother.
Joseph has congenital kyphoscoliosis. In utero, his vertebrae formed differently, which caused both kyphosis, or an outward spinal curve, and scoliosis, a sideways curve. At age 2, Joseph was referred to Scottish Rite for Children where he received expert care from pediatric orthopedic surgeon Amy L. McIntosh, M.D.

When Dr. McIntosh evaluated Joseph, his curve measured more than 80°, which was beyond the point when surgery is recommended. “For young children who have severe congenital curves, bracing or casting doesn’t help because of the abnormal vertebrae,” Dr. McIntosh says. “You have to wait until they’re big enough to surgically fit an implant in them.” Dr. McIntosh monitored Joseph until he was 4. When his curve reached 100°, she recommended six weeks of halo-gravity traction followed by surgery.
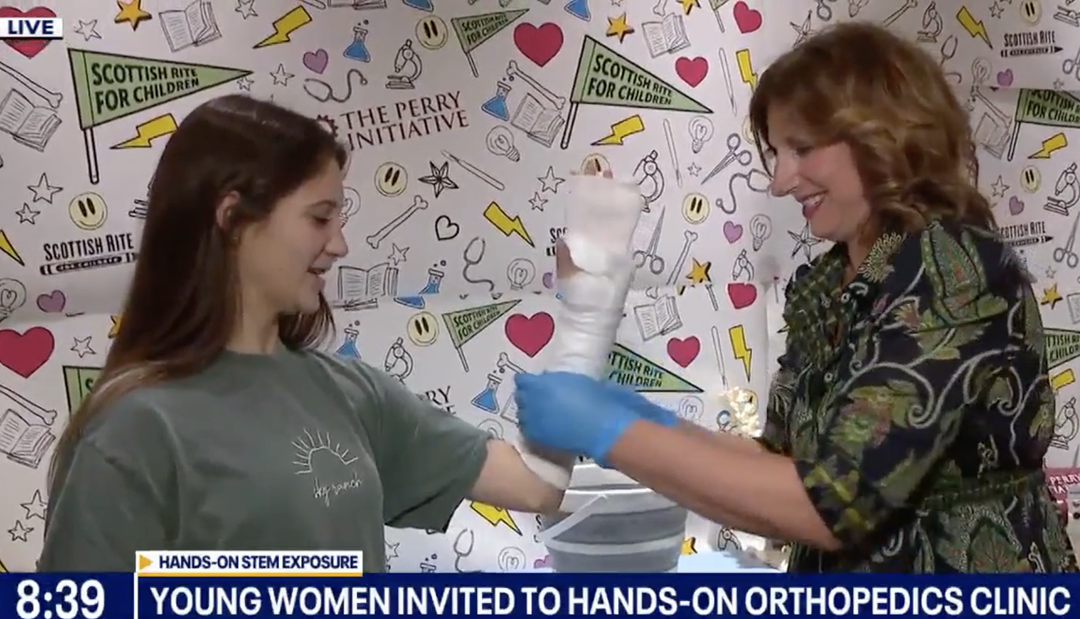
Halo-gravity traction gently stretches and straightens a significantly curved spine in a slow, safe manner. “It’s like taking a spring that’s coiled up and slowly uncoiling it over time,” Dr. McIntosh says. While Joseph was under anesthesia, Dr. McIntosh applied the halo by attaching it to his skull. “I didn’t even feel it,” Joseph says. “It was super magic!” With the help of his care team, Joseph could fasten his halo to a traction device on a pulley system that connected to his walker, wheelchair or bed.
While in traction, Joseph participated in therapeutic recreation, physical therapy (PT) and fun activities in Child Life. “He made friends with everyone, especially the security officers,” Randi says, “and he loved growing his muscles in PT, so he could keep his new friends safe. Scottish Rite became our second family, a home away from home.”
When traction was complete, Joseph underwent surgery. Dr. McIntosh inserted a magnetic growing rod, also known as the MAGEC® System, on one side of his spine and a sliding traditional growing rod on the other side. After a successful procedure, his curve measured 42° — a correction of almost 60%. “He got almost two inches taller,” Dr. McIntosh says.

Going forward, the rods in Joseph’s back will be lengthened as he grows. Rather than undergoing multiple surgeries, an external magnetic device will be used to locate the magnet inside the rod to lengthen it. “The magnetic rod acts as a motor to drive the traditional rod that will slide,” Dr. McIntosh says. This hybrid construct will control the correction of Joseph’s spine until he stops growing and ultimately receives a definitive spinal surgery. “Joseph’s care has been top-notch,” Randi says. “Dr. McIntosh is absolutely the best, a true godsend.”
On his last day at Scottish Rite, Policeman Joseph made his final rounds, protecting the kids and doing a celebratory safety dance on his way out.
Read the full issue.