After an ACL Injury: Physical Therapist Explains Quadriceps Strengthening Progression
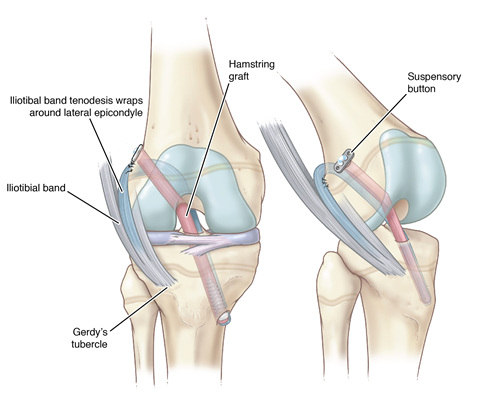
The anterior cruciate ligament (ACL) is a supportive structure inside the knee joint. After it is injured, there are many important areas to focus on during recovery including range of motion, flexibility, strength, balance and core strength. Each of these areas, as well as mechanics with running, jumping, sprinting and cutting, must return to normal before returning to sports.
One area that requires extra attention during recovery is the quadriceps (quad), a group of muscles on the front of the thigh extending to the knee. Due to an injury and after surgery, the body’s response is to “turn off” the nerves to the quadriceps muscle.
What is persistent quadriceps weakness?
Some athletes have quadriceps weakness, and this takes longer to get stronger than other muscles. Unfortunately, this weakness can last years, and bodies will find ways to compensate for quadriceps weakness. However, you may be able to do activities like running and jumping while still having poor quad strength. This is because your hips and ankles are able to compensate, which “hides” quadriceps weakness. This continued weakness can change the way the knee is loaded when running and jumping, which might stress the joint over time.
What is the best way to strengthen the quad muscle?
“There are ways to strengthen the weak quad muscle in isolation,” Physical therapist Jacob Landers, P.T., D.P.T.,O.C.S., CSCS says. “Using a knee extension machine is the most efficient exercise for strength training.” Ideally, strength training should occur three times per week.
- Set the weight to a challenging amount and attempt as many reps as possible.
- Try to do a full set with both legs and then repeat the exercise with one leg.
- If you can do more than 10 reps, add more weight and try again.
- Repeat this process until the maximum number of reps you can complete is less than 10. This will be your starting weight.
.jpg?width=350&height=314)
What comes next?
“Once you have built a base of quad strengthening throughout the first couple of months, work on training different aspects of strength, such as explosiveness and deceleration,” Landers says. Work on performing this quadriceps exercise at faster speeds or performing the lowering phase of the exercise more slowly. Ask for guidance from a strength and conditioning coach or physical therapist for other variations.
This training should be part of a comprehensive program for athletic readiness. Want to know how you can work with our team at Scottish Rite for Children? Read about our bridge program and sign up today!