Get to Know our SRH Staff: Anthony I. Riccio, M.D.
I earned my undergraduate degree from Dartmouth College in Hanover, New Hampshire and attended medical school at Georgetown University School of Medicine in Washington, D.C.
You had an internship at National Naval Medical Center General Surgery – can you explain your time and training there?
In the 1990’s and early 2000’s, orthopedic residents were still required to complete a one-year general surgery internship prior to beginning their orthopedic training. As I attended medical school under the support of the Naval Health Professions Scholarship Program (HPSP), I was required to complete that intern year in a military medical facility. Since NNMC was right up the road from Georgetown (where I had attended medical school and where I would be completing my orthopedic residency), it seemed like the perfect place to do my internship.

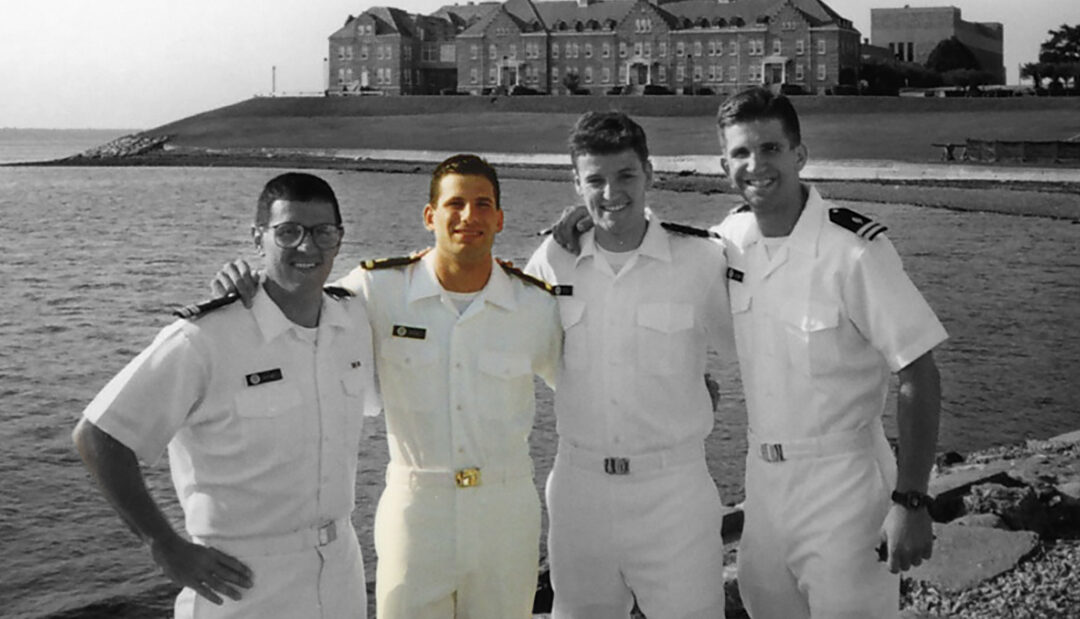
I was commissioned in 1995 and discharged in 2010, so technically I was in for 15 years. Most of this time was spent on Inactive Ready Reserve, while I completed my medical education and training. I was on active duty for five years altogether: one as an intern and four as an attending surgeon.
My Navy time impacted me in many ways, but more than anything, I learned the true value of being part of something that was far bigger and more important than myself. I served during the Iraq and Afghanistan wars and took care of countless wounded warriors, all of whom made incredible sacrifices for our country, our freedom and our families.


I initially wanted to become a college professor to teach and study moral and epistemological development during adolescence. I was advised by my college mentor to do this through the route of medical school and then psychiatry.
I think it’s the dream of every former fellow to one day have the opportunity to return and work at Scottish Rite Hospital alongside those staff who mentored and supported us throughout fellowship. But in all honesty, I never thought I’d be one of the few who was given that opportunity. Dr. Herring was aware that a huge part of my clinical practice with the Navy was caring for service men and women with war related extremity trauma. As my naval commitment was winding down, he called one day and asked if I’d consider coming back to apply the knowledge I’d gained towards managing and researching pediatric orthopedic trauma. As far as I know, no one had ever said no to Dr. Herring and I wasn’t about to be the first!
How long have you worked at Scottish Rite Hospital?
Almost 10 years as staff.
What are your specialties?
Though I started out focusing exclusively on pediatric orthopedic traumatology, my practice has shifted over the years and my current interests include clubfoot along with other infantile foot deformities as well adolescent/young adult foot and ankle deformity.
How do you help your patients feel comfortable and confident?
I really don’t do anything special. I just be myself – not just with patients but with everyone. When patients, parents and colleagues know that they’re getting the “real you” in every situation, it eliminates barriers to communication, puts folks at ease and allows for an open and honest interchange of thoughts and concerns.
What is your favorite part of your job?
Teaching residents and fellows.
What was your first job?
My first job was as pediatric orthopedic surgeon at Naval Medical Center San Diego.
Tell us something that might surprise us about you:
I’ve been on Saturday Night Live multiple times. Take a look at some re-runs from the late nineties through 2007 or so, chances are you can find me.



