Prenatal Care for Clubfoot – What Expecting Moms Need to Know
Our team in the Center for Excellence in Foot led by Anthony I. Riccio, M.D., meets with parents whose babies are diagnosed with clubfoot prenatally and begins treating these children quickly after they are born, beginning interventions within one to two weeks of birth. Learn more about what to expect during the clubfoot treatment process below.
What is clubfoot?
Clubfoot is a congenital (from birth) disorder in which the foot points down instead of straight and turns in, pointing toward the opposite leg. Clubfoot is one of the most common pediatric musculoskeletal conditions that requires treatment by a pediatric orthopedic surgeon.
A clubfoot is not a normal foot that is just twisted and turned into an abnormal position. The outward deformity is created by structural differences inside the foot. The method of treatment for clubfoot cannot alter the structural differences inside the foot. The treatment method takes the structurally abnormal foot that is in an abnormal position and puts it into a series of casts, which slowly turns the foot until it is in a normal position.
If left untreated, clubfoot will make shoe wear problematic and can lead to serious problems, severely limiting activities and even causing difficulty walking.
Prenatal Clubfoot Care: 20 weeks to 40 weeks gestation
Clubfoot can be diagnosed in unborn babies during the mother’s 20-week ultrasound in which the obstetrician or maternal fetal medicine physician reviews anatomy. During this ultrasound, if one or both feet appear to be abnormal, the doctor will refer the mother to visit with an orthopedic specialist to discuss treatment options.
The first appointment with our clubfoot expert Anthony I. Riccio, M.D., consists of a one-on-one conversation about clubfoot and how it is treated. In this appointment, Riccio answers questions that parents have about the condition and educates them on what to expect. This can greatly help a family feel less anxious about the future of their baby and assuage fears about any future disability.
Newborn Clubfoot Care: 1 to 2 weeks old to 2 months old
Riccio encourages families to spend a few days at home enjoying their newborn and then calling Scottish Rite for Children for an evaluation. Ideally, treatment for clubfoot will begin with the first couple of weeks of the baby’s life.
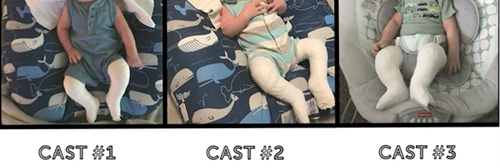
Typical treatment for clubfoot in newborns consists of the Ponseti method, which uses a series of casts and then braces to correct a baby’s clubfoot and prevent its recurrence. In newborns, the first step is to determine the severity of the condition and begin casting.
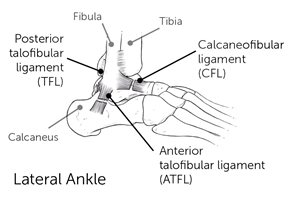
In serial casting, a cast is applied to the foot or feet once a week for three to five weeks. This brings the foot from upside down and turned inward position to a right side up and turned outward position. In some cases, a simple procedure under local anesthetic is performed to release tightness in the Achilles tendon and bring the foot into a normal position. After three to five weeks of progressive casting, a final cast is applied to hold the foot in the normal position for three weeks.
Infant Clubfoot Care: 2 months old to 7 to 12-months-old
After serial casting is completed, the next phase in clubfoot treatment is bracing to maintain the correction that was achieved through casting. Babies will wear a brace called a boot and bar brace consisting of soft silicone lined shoes with soft suede straps. These shoes are connected to each other by a bar to keep the feet turned outward.
Scottish Rite follows the protocol set by the International Clubfoot Congress of wearing the brace for 23 hours a day until the baby is beginning to pull up to stand, which usually happens between 7 to 12 months of age. Bracing does not interfere with the baby’s ability to reach developmental milestones, such as rolling over, sitting independently or crawling.
Toddler Clubfoot Care: 7 to 12 months old to 4 years old
After the baby begins pulling up to stand, wearing of the boot and bar brace is transitioned to nighttime only until the child reaches age 4. If bracing is not done in its entirety, the risk of clubfoot recurrence approaches 100%.
According to research at Scottish Rite, 70-80% of children will not require further treatment after the Ponseti method. Unfortunately, because clubfoot is a structural, congenital difference, approximately 20% of children will relapse and need further treatment, despite the medical providers and families doing everything correctly.
While clubfoot care may seem daunting, it is a safe and pain-free process that will give your baby the best outcome and prevent them from having difficulties later in life. Our team in the Center for Excellence in Foot stay with our patients and families every step of the way.
Learn more about clubfoot.