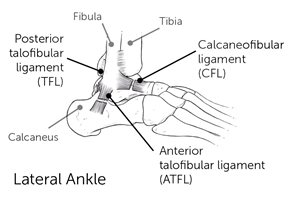
- The anterior talofibular ligament (ATFL) is the more anterior of the two and connects the fibula to the talus (ankle bone).
- The calcaneofibular ligament (CFL) is the more posterior of those two and connects the fibula to the heel bone.
To test for stability, individually assess the function of each of these ligaments with an anterior drawer test.
Seated Assessment – Anterior Drawer Test in dorsiflexion and plantarflexion
Dorsiflexion places the CFL on maximum stretch and plantarflexion places the ATFL on maximum stretch.
- Cup the heel.
- Grab the ankle bone with your thumb while supporting the tibia.
- Bring the ankle into dorsiflexion. *
- Pull forward on the foot and the heel bone while pushing back on the tibia or leg bone.
- See if there is excessive anterior translation through the ankle joint.
* Repeat the test but with the ankle in maximum plantarflexion.
Children without connective tissue disorders will only have ankle instability on one side, typically due to multiple injuries and sprains. Always compare the amount of translation from the bothersome ankle to the normal ankle to assess for any difference.
Assessment of Anterior and Posterior Ankle Impingement
An anterior ankle impingement is typically the result of a dysmorphology of the ankle joint, typically the talus. We see this frequently in children who have had prior interarticular surgeries, particularly those with clubfeet. Their ankle, which is supposed to be a relatively rounded joint becomes more flattened and can’t roll under the tibia bone. Instead it’s flat and as they try to advance the tibia over their foot in walking, the front of the ankle bone bumps and bangs into the front of the tibia bone.
Seated Assessment – Anterior Ankle Impingement
- Palpate for tenderness around the anterior aspect of the ankle.
- Perform forceful maximal dorsiflexion to see if that forceful abutment of the talus into the tibia reproduces anterior ankle pain.
With posterior ankle impingement, some children will have an os trigonum which is normal ossification (bone growth) behind the talus bone. The vast majority of these are completely asymptomatic, but occasionally it can be large enough or the child can be active enough that the ossicle will bang against the back of the ankle during points of maximal plantarflexion. This is commonly seen in gymnastics and dancers who spend a lot of time up on their toes. Because they are repeatedly, maximally plantarflexing their ankle, they can force the ossicle into the posterior aspect of the joint which can create pain.
Seated Assessment – Posterior Ankle Impingement
- Palpate for tenderness around the posterior aspect of the ankle.
- Forcefully plantarflex the ankle to see if we can reproduce posterior ankle pain.
Assessment for Overuse Conditions
Sever’s Disease
Calcaneal apophysitis, or Sever’s disease, is a type of overuse injury caused by repetitive movements. It is the most common cause of heel pain in active children ages 8-12. This is often seen with tightness in the gastrocnemius, and the growth plate, the calcaneal apophysis becomes inflamed.
Seated Assessment – Palpation of the Calcaneal Apophysis
- Examine the insertion of the Achilles tendon in the area of the calcaneal tuberosity.
- Slide your thumb off the very back of the heel.
- Approximately 1 – 1.5 centimeters forward.
- Push and squeeze on both the inside and outside of the calcaneal tuberosity, this will reproduce the pain in children with Sever’s disease.
Plantar Fasciitis
More often seen in adults, children and adolescents may also experience this tightness and pain on the plantar aspect of the foot. Oftentimes it doesn’t stop a child from doing the activities they want to do, but it becomes bothersome after they’ve stopped their activities and sit down or are taking a car ride or get out of bed first thing in the morning.
Perform a Silverskiold test to assess plantar fasciitis because it is directly linked to tightness of the gastroc soleus complex.
- Take the big toe and dorsiflex it as much as possible.
- This puts the plantar fascia on stretch because of some attachments to the flexor of the big toe.
Often passively dorsiflexing or extending that big toe will be enough to set these children off if they have a fasciitis in this area. If not, it certainly allows us to really get a sense of how tight that plantar fascia is and directly palpate it to see if it is painful for the child.
Kids and Insoles: An Introduction to Orthotics
Kelsey Thompson C.P.O., L.P.O.
Orthotist Perspective
What should you look at first?
- Look at what shoes the patient presents with.Are they supportive shoes or flexible/non-supportive shoes?
- Ask if those are the most commonly worn shoes, or if they have others.
- Ask when the patient has pain.
- With shoes, barefoot, all the time?
- Do any shoes make their pain improve?
- Have they tried better shoes or any off the shelf insoles?
- If so, what have they tried?
Shopping for Shoes
Proper sizing is important.
- The quality of shoes is better in adult sizes versus kids’ sizes.
- Kids shoes are sized off Men’s sizes.
- 5Y is a 6.5 Women’s, so girls can get into women’s shoes quicker than boys.
- Women’s – B width, Men’s – D width.
Price
- Price can be directly related to quality but not when it comes to popularity.
- Related to quality of cushioning and how long shoe will last, not support.
- Number of miles and still have the same amount of cushioning.
Where to Shop
- Specialty running shoe stores (Run On, Frisco Running club, etc.) are recommended.
- Can get past year models online for less.
Adding Support
- Arch support needs to come from an insole bought separately.
- A severe pronator needs motion control or stability shoeDenser midsole material on medial side of shoe.
- Offered by Asics, Brooks and New Balance Shoes.