Key messages from Joseph (I-Yuan) Chang, M.D., and a panel discussion by pediatric orthopedic and sports medicine surgeon Henry B. Ellis, M.D., and Gerad Montgomery, B.S.N., FNP-C, at Coffee, Kids and Sports Medicine.
Watch the lecture
Print the PDF
How Advances in Radiographic Imaging Can Protect Patients
Though digital X-rays are the gold standard for many musculoskeletal evaluations, EOS is a relatively new technology designed to achieve results with less radiation. These devices are well-suited for pediatric orthopedics because many treatments, like lower extremity and spine straightening procedures, require periodic imaging to monitor growth and success over time.
Here are several features of how EOS is the best option for some evaluations:
- Uses very low-dose radiation – uses 1/7 the amount of radiation, compared to traditional X-rays
- Facilitates accurate assessment of standing alignment – evaluating alignment while a patient is weight-bearing posture provides a more accurate picture of the interaction between the joints of the spine, hips and legs.
- Creates a single image immediately – with a traditional X-ray, separate films in supine or standing are “stitched” together. This process can be negatively affected by human error (this is done relatively quickly by using computer software at a work station, but may be done incorrectly due to inexperience or carelessness).
IMPORTANT NOTE: It does require a child to stand still for a short period of time, so can only be used when the patient is able to bear weight and can stand still for approximately 10 seconds.
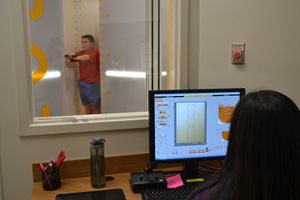
Scottish Rite Hospital has been using the EOS Imaging System since 2016 and had a second system installed with the opening of the Frisco campus in 2018. As pediatric providers, we are committed to using the lowest dosage of radiation possible for studies. EOS has been a useful tool in caring for patients with spinal deformities, lower extremity limb differences and malalignment.
Ordering and Reading Pediatric or Adolescent Elbow X-rays
These tips can be helpful with other X-rays. Watch the full lecture to see how they are applied to ordering and reading an elbow X-ray.
Tips for Ordering X-rays:
- Always order two perpendicular views – X-rays are 2-dimensional. To evaluate a 3-dimensional object, a bone or joint, two views are necessary. In most cases, the anteroposterior (AP) view and the lateral (LAT) view will suffice.
- When reading a radiology report, remember that the radiologist does not have the advantage of the complementary physical exam. This is critical to pair with the reading of the imaging. When placing an order, include a note about the clinical exam in the order to provide context for the radiologist.
Tips for Reviewing X-rays:
Joseph Chang, M.D., pediatric musculoskeletal radiologist offered “five easy steps” to reading an X-ray.
- Is there a positive ‘fat pad sign’? A fat pad sign, also known as a sail sign, is a sign of a joint effusion. A joint effusion is an imaging finding that is highly predictive of radiographically occult injury in the joint. A pediatric elbow has so much more cartilage than an adult, making certain injuries invisible on radiographs.
- Is the alignment normal? In the elbow, assess the anterior humeral line (lateral view) and radiocapitellar line (AP and lateral view). Disruptions to these lines are signs of a fracture or dislocation and need to be treated.
- Are the ossification centers normal? Ossification centers have a strict order of appearance and disappearance – if one is missing or out of place, an injury may have occurred. The acronym “CRITOE” can be used to help recall the growth plates in the elbow but knowing to look for them is a good first step. Because growth disturbances can be prevented with proper management, refer to a pediatric orthopedic specialist when you are unsure.
- Is there a subtle fracture? Evaluate the metaphysis of the bone. The bony cortex should have a nice, smooth slope. Children have soft and more flexible bone, therefore the bone sometimes buckles instead of breaking. These injuries may appear as a blip on the X-rays.
- CLINICAL TIP: Be careful not to miss a buckle fracture (also known as torus fracture or incomplete fracture) in your imaging review when a patient has these symptoms.
- Wrist AND elbow pain
- Loss of terminal extension and pronation/supination
- Pain over the radial neck
- Did you consider the normal variants? Before you finalize your diagnosis, take a step back and see if what looks abnormal is a normal, developmental appearance in a growing child. Skeletally immature patients may have radiolucent growth centers composed of cartridge and sometimes bone. Secondary ossification centers (i.e. trochlea, lateral epicondyle) can have irregular margins or appear as separate ossicles, mimicking traction stress injury or fractures.
“I think that a practitioner correlating a good clinical exam with the first three steps above will help you identify 90% of elbow injuries and fractures in this population” says Henry B. Ellis, M.D., pediatric orthopedic surgeon.
Joseph (I-Yuan) Chang, M.D., is a radiologist with specialty experience in pediatric musculoskeletal radiology practicing at Scottish Rite for Children Orthopedic and Sports Medicine Center. He completed his training at the University of Cincinnati College of Medicine followed by a residency at Cleveland Clinic Foundation.
The radiology staff at Scottish Rite Hospital participates in interactive, preoperative and postoperative conferences with the pediatric orthopedic specialists. Imaging services include X-ray, EOS, musculoskeletal ultrasound, CT and state-of-the-art MRI capabilities on both campuses. They offer on-demand consultations for our team to support high quality and efficient care.