Return to Weight Lifting: A Guide for Young Athletes After Injury
Patients in the Scottish Rite for Children sports medicine clinic may lift weights as part of their primary sport training or with a strength and conditioning coach to supplement sport-specific training. When an injured athlete is released back to activities that include weight lifting, Scottish Rite for Children athletic trainer Allen Tutton, M.S., L.A.T., A.T.C., C.E.S., provides systematic instructions to ensure a safe, progressive return to training. Tutton is uniquely qualified with skills as both an athletic trainer and a corrective exercise specialist (CES). A certification from the National Academy of Sports Medicine, the C.E.S., requires a solid understanding of the interrelationship of movement quality and exercise, a must for strength and conditioning advice for young athletes. Here are his tips for safe weight lifting:
Before You Start
- Focus on form and technique instead of the amount of weight or number of repetitions.
- Increase your working weight slowly after an injury or a long break from training.
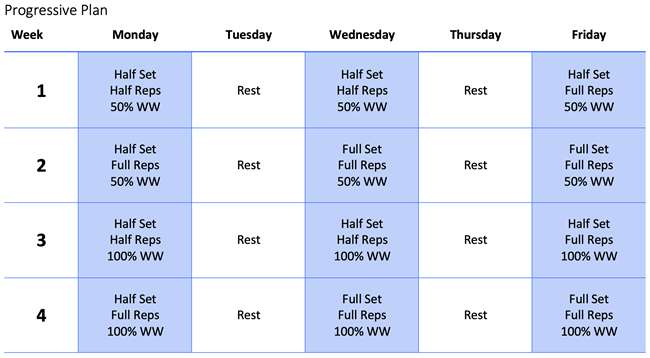
- Working weight (WW) is the repetition (not max) weight used in your workout on a normal day.
Warm-up and Lifting
- A warm-up is necessary to help you perform your workout at your best.
- An optimal, dynamic warm-up includes upper and lower body stretches as well as light jogging.
- Have a spotter with you when you begin lifting.
- If you feel any abnormal discomfort, you must stop and rest 48 hours before trying the step again.
- If your working weight is too heavy, decrease the weight used.
Terms to Know
- Repetitions (reps) = number of times you perform the exercise before a rest.
- Set = number of times you repeat the exercise and rest.
Wrap It Up
- Each workout should not last longer than one hour.
- Stay hydrated and rest at least 24 hours between sessions.
Managing Load: Preventing Overuse Injuries
Load can be measured in several ways:
- Total work or repetitions done in a day.
- Total weight lifted in a day.
- Collection of work throughout a period, such as a week or a month.
Rushi Patel, P.T., D.P.T., SCCE, says, “A combination of how much weight is lifted, how often and for how long can all play a role in potential overuse injuries in the weight room.”
Patel offers these tips to minimize the risk of injuries:
- All sport-related training should be considered part of the overall load. Times to reduce the weight or intensity of a weight-lifting routine include:
- Starting a new sport or returning to sport after a break.
- Preseason sport-specific intense training.
- Focused sport-specific training in a camp or when learning a new skill.
- Monitor how you feel in the first 24-48 hours after a workout. Excessive joint pain or soreness that lingers might be a sign to modify some activities related to your workouts.
To learn how nutrition can play a role in safe and effective strength training programs, read this article.

Nutrition Tips for Young Athletes in Stop-and-Go Sports
Alternating periods of intense power and speed, with short or long periods of rest, involve all of the major energy systems in the body. Therefore, meals and snacks throughout the day for these athletes should include appropriate mix of all foods and nutrients.
“It’s easy for busy young athletes to not make food a priority, showing up for practices and games under fueled and thinking they can power through”, says certified sports dietitian Taylor Morrison, M.S., R.D., CSSD, L.D. “However, the reality is that food and nutrition are very important components to optimal performance and injury prevention. The good news is that this food and nutrition doesn’t have to be complicated. An athlete can incorporate simple meals, snacks and fluids throughout the day using some general guidelines thereby reducing concerns and optimizing health and performance”.
CONCERNS FOR THE YOUNG ATHLETE IN STOP-AND-GO SPORTS
Burning Out Early
Because of the intensity of some stop-and-go sports (like basketball, soccer, tennis and hockey) and because of the length of some games (like baseball or football) and tournaments (like basketball, soccer, tennis and volleyball), young athletes can use up their energy stores before the event is over. This especially becomes a problem if the athlete has not eaten a proper meal or snack earlier in the day or prior to the event and does not bring appropriate snacks for during the event.
End of the Season Injury
If this pattern of burnout continues, the constant fatigue during events can put the athlete at increased risk of injury due to decreased motor skills and performance. Poor nutrition or under-fueling can also lead to a lack of important nutrients like protein, fat, iron, calcium and vitamin D, which can also increase an athlete’s risk of injuries like stress fractures.
Dehydration
Dehydration is another contributor to fatigue, but also a cause of headaches and muscle cramps in the young athlete. Either of these can lead to decreased performance and injury. Of special concern are those young athletes playing in the heat or with extra gear like football, softball and hockey. Dehydration in these young athletes can lead to heat illness if it is not properly recognized and addressed.
NUTRITION SOLUTIONS FOR THE YOUNG ATHLETE IN STOP-AND-GO SPORTS
Proper Fueling Before and During Events
Eat a balanced meal at least three to four hours prior to the event and a small snack just before. Make sure to offer easy-to-digest carbohydrates to keep energy levels up until the very end of games and tournaments. More popular suggestions are fruit slices, dried fruit, crackers, pretzels, fig bars or sports drinks.
Balanced Meals Throughout the Day
Remember that the exact amount of food and nutrients needed vary depending on gender, height, weight, stage of development, sweat rate, sport played and position played. However, overall a young athlete’s plate should consist of:
- Variety of Carbohydrates – Mix it up with sources like milk and yogurt, whole grains, fruits and starchy vegetables. Carbohydrates provide short and long-term energy to fuel for a practice, game or tournament.
- Lean protein – Protein is important to repair any torn muscles and build tissue.
- Healthy fats – Fat is important for the growing brain and has potential anti-inflammatory benefits.
- Healthy fats, such as mono- and polyunsaturated fats, are important for brain development and function, aid in the absorption of vitamins A, D, E, and K and may have anti-inflammatory benefits. Learn more about healthy fats for the young athlete.
Getting carbohydrates, protein and fat from a variety of sources ensures that the athlete is also getting proper amounts of other nutrients like calcium, vitamin D and iron, among many others. Eating enough calories from carbohydrates, protein, fats and these nutrients helps promote optimal recovery and prevents injuries.
Hydrate
Drink fluid consistently throughout the day. Most of the time, an athlete should choose water and milk. Make sure to bring plenty of water to events adding a sports drink (for electrolytes and carbohydrates), if needed and encourage sips during timeouts, breaks and halftime. For heavy sweaters, salt can be added to drinks or salty snacks can be incorporated into breaks and halftimes.
Visit our sports hydration page to learn more about nutrition and fueling the young athlete.

Young Athletes and Heel Pain
What are growth centers?
The medical term for a growth center is a physis. The physis is an area of the bone that has soft tissue called cartilage that is later replaced by new bone cells. Some are areas where bone growth makes bones longer. Others, called apophyses, give the bones a unique shape. These growth centers are found in the elbow, pelvis, heel and other areas. The apophyses are attachment sites for tendons.
What growth center is in the heel?
The calcaneal apophysis is in the calcaneus (heel bone). The apophysis is the attachment site for the very strong tendon from the calf muscle, called the Achilles tendon.
What causes heel pain in the calcaneal apophysis?
Children become more committed to sports around 8-12 years old. With running, or repetitive jumping, the Achilles tendon pulls on the cartilage in the heel. This, accompanied by the impact on the ground with running and jumping, can lead to irritation in this area. Because this has a gradual onset, this is referred to as an overuse injury and is often referred to as Sever’s disease.
What is Sever’s Disease?
Sever’s disease, or calcaneal apophysitis, is a type of overuse injury and the most common cause of heel pain in active children ages 8-12. It is caused by repetitive movements, like running and jumping and may occur in only one or both sides. The pain is usually not related to a specific injury and comes on gradually.
What is the treatment for Sever’s disease?
Changing shoes or adding heel cups may be recommended to help with comfort during recovery. Simple ankle stretching exercises may also be helpful. Other treatments are available and should be considered on an individual basis, but rest is the most common prescription for this condition. Returning to a sport and other physical activity may gradually prevent recurrence. Pain may last months to years and may come back or worsen with increased sport or activity.
How long does Sever’s disease last?
Sever’s disease will resolve with completion of growth in this area. Because the growth plate is soft until it is closed, this problem can happen again in this age group. Pain in this area typically resolves by the mid-teenage years.
What factors may increase risk of initial or recurrent Sever’s Disease?
- Playing sports on a hard surface or barefoot.
- Footwear with poor cushioning, such as soccer cleats.
- Year-round sports participation.
- Sudden increase in training intensity.
- Increase in duration or frequency of activity, such as tournaments and camps.
- Tight Achilles tendon or calf muscle.
Learn more about Sever’s disease in this popular short lecture featuring sports medicine physician Jane S. Chung, M.D.

Jacob C. Jones, M.D., Joins the Sports Medicine Team at Scottish Rite for Children
Before completing his fellowship at Boston Children’s Hospital/Harvard, Jones attended medical school at the University of Missouri, where he earned his doctor of medicine. He completed his pediatrics residency at Children’s Medical Center/UT Southwestern Medical Center in Dallas and received additional specialty training at Boston Children’s Hospital, with fellowships in sports medicine and sports medicine/musculoskeletal (MSK) ultrasound. Jones rotated with the Scottish Rite Sports Medicine department during his residency.
“Scottish Rite is known both locally and nationally as a leader in pediatric orthopedics and sports medicine,” says Jones. “I am excited to be back in Texas with an opportunity to help young athletes get back to doing what they love.”
“North Texas is the place to be when it comes to youth sports,” says Scottish Rite President/CEO Robert L. Walker. “Dr. Jones’ expertise will be a great addition to our team in Frisco. We are very proud to have him join our staff.”
Jones is board certified by the American Board of Pediatrics in Sports Medicine and Pediatrics. He is a member of American Medical Society of Sports Medicine, American College of Sports Medicine, American Academy of Pediatrics (AAP), American Medical Association and Pediatric Research in Sports Medicine Society.