At the Forefront of Innovation: Spinal Surgery at Scottish Rite for Children
Hearing that your child needs spinal surgery for scoliosis brings a flood of questions and a lot of uncertainty. Using the newest technology and innovative methods, the experts at Scottish Rite for Children are some of the best pediatric orthopedic surgeons in the world. Our leaders support your child throughout treatment, making their spinal surgery a success from start to finish.
We provide a multidisciplinary, patient-centered approach to scoliosis treatment. Spinal maturity; the degree, extent and location of the curve; and the potential for progression are all considered when determining treatment.
Types of Scoliosis
- Adolescent idiopathic scoliosis (AIS) – the most common form of scoliosis that occurs in children ages 10 to 18
- Congenital scoliosis – scoliosis that is present at birth and is due the intra-uterine formation of abnormally shaped/formed vertebrae
- Early-onset scoliosis – scoliosis that occurs before the age of 9
- Neuromuscular scoliosis – secondary scoliosis that develops because of an underlying medical condition that adversely affects the brain, nerves, or muscles
- Syndromic Scoliosis: An underlying genetic syndrome that causes the scoliosis
Additionally, scoliosis can be categorized by the following:
- Thoracic scoliosis – curve in the middle, or thoracic, part of the spine
- Lumbar scoliosis – curve in the lower, or lumbar, part of the spine
- Thoracolumbar scoliosis – curve in both the spine’s lower thoracic and upper lumbar parts
When Surgery is Needed for Scoliosis
Depending on the child and the severity of their curve, surgery may be the best treatment option. While not all cases of scoliosis require surgery, the following factors are an indication that surgery is needed:
- Your curve is greater than 50 degrees, and/or
- You have significant growth remaining
- Your curve progressed to 50 degrees despite compliance with brace wear
- You have a underlying neuromuscular or syndromic condition.
The most common type of surgery performed for scoliosis is a spinal fusion. In a spinal fusion, the curved vertebrae are fused together to create a single, solid bone. This stops the growth in the abnormal part of the spine and prevents the curve from worsening. Metal rods attached by screws, hooks or wires are used to hold the spine in place until the bone heals. In all spinal fusions, a bone graft is used to help promote the fusion and the bones grow together to create one solid bone.
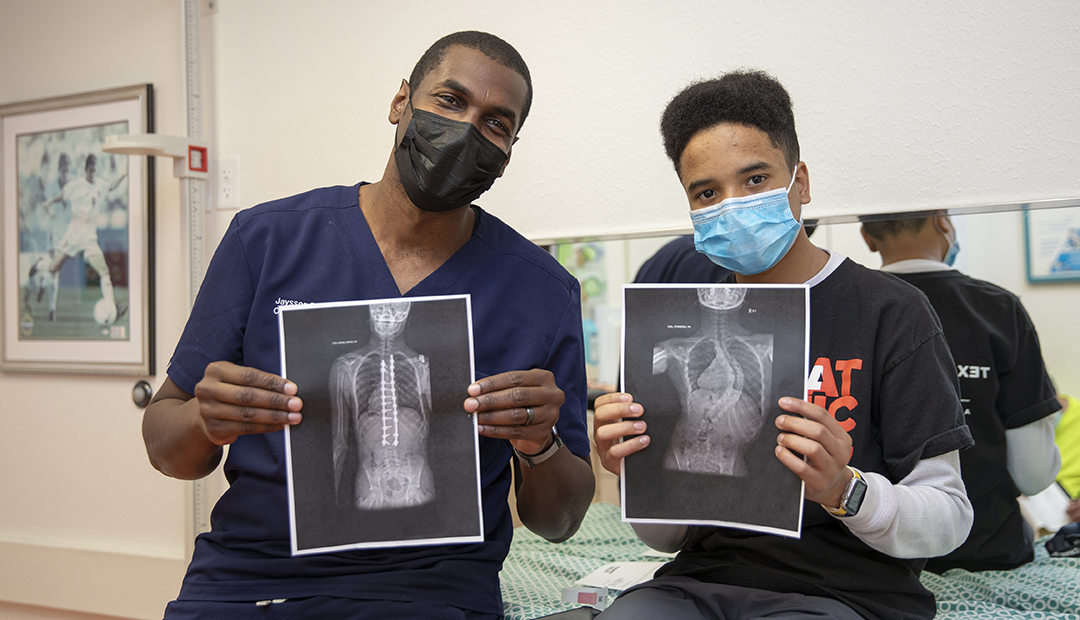
Having Spinal Surgery at Scottish Rite
Led by Daniel J. Sucato, M.D., M.S., our Center for Excellence in Spine employs six pediatric orthopedic surgeons who specialize in spinal surgery for scoliosis. Our diverse team of surgeons works together to create individualized treatment plans for each patient and ensure that the child and the family know what to expect each step of the way. Multiple departments work together to provide a multidisciplinary approach to care and treatment. Orthopedics, Psychology, Physical Therapy and more will address all your child and their needs to ensure they are prepared for surgery. Our psychologists help our patients cope with having surgery and address their feelings about their procedure, giving children the opportunity to express their emotions. Following surgery, our team works with your child to make recovery as easy as possible.
Tackling the Most Complex Cases
New and innovative techniques allow our experts to tackle the most difficult cases. This includes Magnetic Expanded Growth Rods (MCGR), Halo Gravity Traction (HGT), Vertebral Body Tethering (VBT), and Posterior Spinal Fusion (PSF). Our experts have experience treating complex cases, such as treating patients with a curve of over 100 degrees.
Road to Recovery
Following surgery, our team begins the recovery process with the patient. Using different pain management techniques. Our physicians are dedicated to seeing each patient through their recovery.
After a spinal fusion, it is common to need to minimize bending or heavy lifting. Our surgeons will go over limitations and discuss the importance of proper aftercare. Our team works with each patient to determine readiness to return to activities and coaches them through the recovery process.
How to Learn More and Become a Patient
Learn more about our Center for Excellence in Spine and scoliosis treatment.
Learn how to and how to make an appointment with one of our world-renowned experts.




