One of the eight cheerleaders ran across the mat to do a pass while practicing the routine. But one of the moves was off, she didn’t have the momentum to finish the back flip at the end, and she landed on her head. The group of parents let out a collective gasp before falling silent.
Marie Hunt, a cheer mom and nurse practitioner, rushed into the gym to help the injured cheerleader, who turned out to be her daughter. “Sophie was standing up so my first thought was that it must not be too bad,” the Plano mom says. “She went on to tumble for 30 more minutes.”
A couple of hours after practice, a swollen nose and black eyes prompted Hunt to take the 12-year-old to an urgent care center. They left with the diagnosis of a broken nose.
Nearly two days after the fall, however, disturbing symptoms began to surface.
Hunt left earlier than usual for work and called Sophie to be sure she didn’t oversleep. After the 27th time hearing Sophie’s voicemail message, she called for help. A friend sent her kids to the door. It took Sophie what seemed like forever to answer their repeated knocks and doorbell rings.
Sophie’s out-of-character behavior continued with a barrage of text messages to her mom. “She knows I can’t leave my job, yet she kept asking if I could bring her things she had left at home,” Hunt recalls. “I told the surgeon I work with who then asked if I had considered a traumatic brain injury.”
Hunt would later find out that Sophie had suffered a concussion, and the extra tumbling only worsened the brain injury.
Concussions 101
Concussions are an alarmingly commonplace injury, particularly among kids. According to a recent study in Pediatrics, nearly two million kids suffer concussions each year, and one-third of those happen to kids younger than 12.
A concussion is a mild traumatic brain injury that occurs from a direct blow or jolt to the head. Though the deceleration of the head is sudden, the brain stays in motion, bouncing around or twisting in the skull, causing functional changes in the brain. Symptoms can include headaches, dizziness, confusion and fatigue.
It used to be assumed that young brains had exceptional healing ability. Turns out, those young brains are more vulnerable to the effects of concussions because kids’ brains are still developing, and their smaller and weaker necks and shoulders mean that less force is needed to cause a brain injury.
Youth football has long taken the blame for concussions, especially in the wake of revelations that pro football players suffered permanent brain damage from the abuse they took on the field. But cheerleading, hockey, basketball, martial arts, wrestling, baseball, softball, gymnastics, rodeo, lacrosse, volleyball, swimming and soccer are proving to be just as dangerous.
In fact, soccer accounts for nearly 20 percent of total team-sports concussions (girls’ soccer makes up more than half of that), basketball for almost 10 percent and volleyball for a little more than 1 percent each year.
What’s more, a third of all concussions among kids are caused by non-team activities such as ice skating, snowboarding, skiing, skateboarding, bicycling and falls on the playground.
Six-year-old Courtney McCracken was playing on a Denton splash pad during a day care program when she ran into a pole. Courtney didn’t have a visible bump on her head, so teachers let her continue to play. But after persistent headaches for a week, Courtney’s mom, Cindy McCracken, took her daughter to the pediatrician, who recognized the concussion signs.
Mind the Signs
Not all concussions are the result of a blow to the head either: A child can give her brain a severe jolt just by slamming into a goal post with her shoulders and chest.
“Typically, symptoms are noticed soon after the injury, but we have seen some show up or worsen the next day,” explains Dr. Troy Smurawa, director of pediatric sports medicine at the Children’s Health Andrews Institute for Orthopedics and Sports Medicine in Plano.
He says to watch for signs such as headache, dizziness, sensitivity to light or noise, confusion, fogginess, personality changes, lack of concentration and nausea or vomiting.
Forty-eight hours after Sophie landed on her head, cognitive testing at the pediatrician’s office revealed issues, so she was referred to Children’s Health in Dallas.
Hunt, who once worked as a nurse in the neurosurgical intensive care unit, realized how easy it can be to miss the signs.
“The urgent care doctor missed it, and so did I,” Hunt says. “I thought since she didn’t lose consciousness, a concussion wasn’t a possibility.
That’s actually a pretty common misconception, according to Dr. Ricardo Guirola, pediatric sports medicine physician at Cook Children’s in Fort Worth.
“The old guidelines of diagnosing a concussion is one reason a lot of concussions in the older generation went unrecognized,” Guirola says. And repeated unrecognized concussions could lead to chronic traumatic encephalopathy (CTE), a disease similar to Alzheimer’s and caused by hits to the head. Late NFL players Junior Seau and Tyler Sash were both found to have CTE.
Because diagnosis depends in large part upon self-reported symptoms, it’s important that kids know the warning signs too.
Basically, if your child seems at all off, better to get him checked out. “Parents are the most important partner for physicians,” says Dr. Bert Vargas, director of the Sports Neurology and Concussion Program at the University of Texas Southwestern Medical Center O’Donnell Brain Institute.
Double Header
Smurawa says that it takes 2-3 weeks for about 85 percent of young kids to recover after a concussion — meaning they’re able to return to their normal activities. While rare, a few kids struggle with aftereffects of a concussion such as memory loss, chronic headaches and problems with concentration, which may linger for several weeks, months or even years. And these long-term effects increase if a child has a second concussion. In fact, after a concussion, kids are actually at a higher risk of suffering another concussion before the first one has fully healed, even if they’re hit with less force. The unusual result is called second impact syndrome and causes rapid and severe brain swelling and often results in death.
“From experience and observation, the more concussions a child has, the closer together they are and the younger the child is, the more likely a child is to have long-lasting effects such as difficulty with school and ongoing symptoms such as headache or dizziness,” Smurawa explains.
Dory Sjogren’s daughter, Ella, has been playing soccer since kindergarten, and in November, her Dallas club team played one of the top teams in the city, known to be very aggressive. During the game, 11-year-old Ella turned so the ball would miss her face, and it hit the back of her head instead.
“I didn’t see it, but a dad on our team said her head went forward and snapped back before she went down,” Sjogren recalls.
The league nurse assessed Ella on the field and determined that Ella had enough symptoms to disqualify her from returning to play. Sjogren called the pediatrician that night and was advised to keep Ella off pain medications for the first eight hours to avoid masking her symptoms.
“Since Ella wasn’t heading the ball (hitting the ball with her head) when it happened, it didn’t seem like it could be a concussion,” Sjogren explains. “I just didn’t know.”
Two days after the injury, Ella saw Dr. Shane Miller, sports medicine physician at Texas Scottish Rite Hospital for Children Sports Medicine Center in Plano and associate professor of orthopedics and pediatrics at UT Southwestern Medical Center. Miller assessed the speed and reaction time of Ella’s memory recall and recognition using ImPACT (Immediate Post-concussion Assessment and Cognitive Testing), a computerized neurocognitive test that’s widely used by the medical community. Results revealed a concussion.
Getting Back in the Game
Hunt enlisted a specialist to ensure that Sophie’s initially misdiagnosed concussion didn’t go untreated and lead to more severe problems.
“I think [that some parents] just aren’t informed about the importance of seeing a specialist,” Hunt says. “I know many parents only go to their general practitioner or pediatrician for concussion treatment, and they are not getting the assessment of the brain function by doing that.”
Sophie’s five-week treatment plan included avoiding electronics and loud noises, following an anti-inflammatory diet (limiting sugar), taking supplements such as fish oil and vitamin B, using sunglasses and a hat outside to avoid bright light, staying home from school the first week and attending only half days the second week. At school, she ate lunch in the library, changed classes before the dismissal bell and painted or drew while listening to lessons. Smurawa also says that deep sleep helps the brain to recover and recommended that Sophie get at least 10 hours each night.
“We have found that instead of kids sitting in a dark room to recover, they do better with light physical activity and reading for short intervals about 3-5 days after the injury,” Smurawa says.
A trainer from Greenhill, where Ella goes to school, worked with her, her doctor and her teachers to help her get safely back into the school routine.
Two weeks later, Ella got the OK to return to the sport she loved — slowly. She was allowed to run with the team and work with balls but have no contact with other teammates. The coach decided not to put her in for the final game of the season, and instead she started playing in tournaments a couple of weeks later.
All 50 states have a Return to Play law in place to prevent athletes from returning to the field, rink, ring, court or gym too soon. In Texas, only a physician can clear an athlete, and under Natasha’s Law, passed in 2011, coaches and athletic trainers are required to, among other things, get training on how to react when players sustain concussions. But this only covers middle and high school athletes at public and charter schools (though some private schools and clubs have also adopted the law). Surprisingly, youth sports are not regulated, making the risk of concussions highest among those under the age of 12.
“Parents [should] check with their [school or league] and be sure there is a concussion management plan in place,” advises Miller, who suggests that all parents ask about concussion education and awareness for coaches and other officials and return to play guidelines before letting their child play.
Because despite the law, coaches and trainers drop the ball — oftentimes inadvertently — when it comes to preventing and treating concussions.
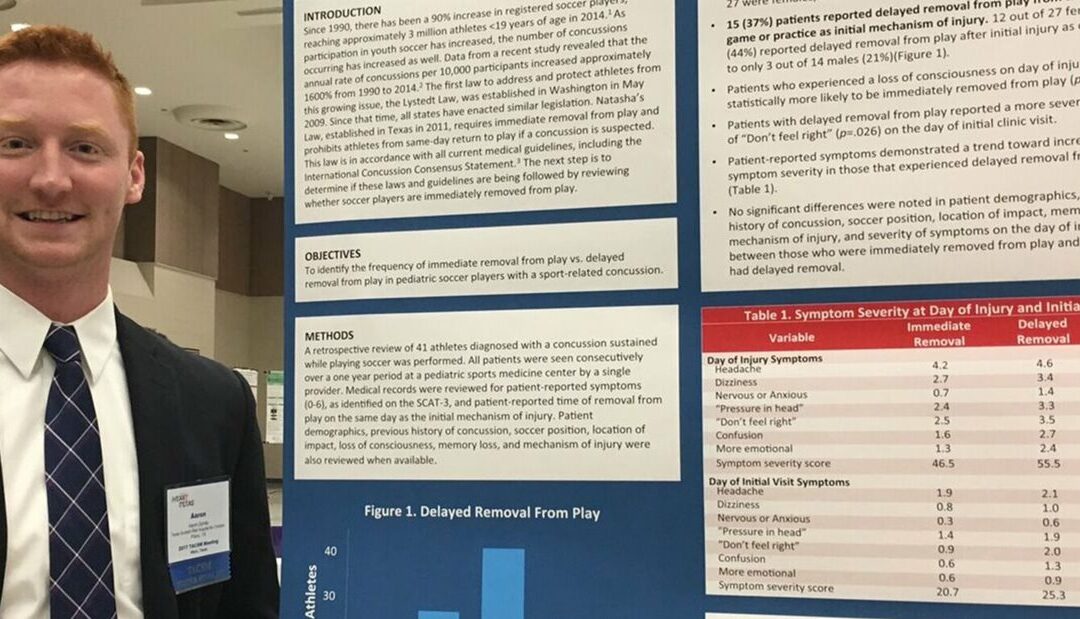
Miller reports that in the last five years, Texas Scottish Rite Hospital has seen an increase in the number of concussions in kids, many of whom had returned to play on the same day of the injury. So he conducted a study and found that more than one-third of patients with concussions continued to play or returned to play on the same day, worsening their symptoms and prolonging recovery.
“Sometimes these kids are going back in the game because of the athlete’s mentality of pushing through, and other times the coaches didn’t recognize the symptoms,” Miller explains.
Playing Defense
By playing safely, consistently checking equipment, following the rules of the game and using proper techniques, young athletes can reduce their chance of suffering a concussion. Smurawa admits that 25 percent of sports-related concussions happen from illegal plays.
Strength training and conditioning before play helps to prevent injuries too. Miller says many concussions happen toward the end of a game when athletes are fatigued and are less able to protect themselves.
Some schools in the Dallas-Fort Worth area do preseason baseline tests to assess an athlete’s brain function before practices begin, but not all ages and sports are included, so ask your doctor.
Cassie McBee’s 12-year-old son, Ethan, plays football at school in Fort Worth. As part of a drill, he was repeatedly hit by another player. After, coaches suspected a concussion and sent Ethan to the school trainer. In the days that followed, Ethan complained about headaches, was unusually sleepy and seemed to be suffering from short-term memory loss.
McBee took her son in for testing. Ethan failed the post-concussion test when they compared the results to the baseline test the school trainers did before the season started, and he was diagnosed with a concussion.
“[A baseline test] is a computerized test that allows us to get a baseline on the athlete,” Guirola explains. “It looks at the balance and brain function so we can compare those results with further testing if a concussion occurs. After the injury, the test helps to determine an athlete’s ability to return to play and to guide their recovery.”
Ethan stayed on the sidelines for nearly three months before being cleared to begin his slow progression back into practice and eventually games.
Sophie was actually the 13th student at her school to get a concussion this year, and though she made a full recovery, her mom wishes she had sidelined her daughter immediately after the fall. The continued rotational motion of tumbling that day only made Sophie’s concussion worse.
“Have any head injury checked immediately,” she cautions other parents. “Had we initially treated it as a possible concussion, Sophie may not have gotten so bad.”.
Read the full article on DFWChild.