


Sports Medicine Team from Scottish Rite for Children Had Strong Presence at PRiSM 2023
The sports medicine team from the Scottish Rite for Children Center for Excellence in Sports Medicine recently attended the 10th Annual Pediatric Research in Sports Medicine (PRiSM) society meeting in Denver, Colorado. Several of our team are founding members in this group leading the way in pediatric sports medicine research.
Medical director of clinical research Henry B. Ellis, M.D., says, “Most conferences are designed to gather one discipline, but this one is inclusive. Scottish Rite had an impressive presence not only in attendance, but also with most of the 23 staff who attended actively contributing.” The Scottish Rite team included sports medicine physicians, pediatric orthopedic surgeons, a radiologist, advanced practice providers, physical therapists, researchers, psychologists and more. Many of them presented and led discussions about important care and treatment techniques for young athletes.
The three-day meeting included a variety of formats for collaboration and learning. Our team presented results from studies at the podium and during poster sessions where authors held conversations with attendees about the projects. The program also included a variety of didactic sessions designed to inform the participants of available evidence on a topic while stimulating discussion for future research.
Some of the noteworthy accomplishments of our team include:
- Our director of Movement Science Sophia Ulman, Ph.D., had an active role in multiple aspects of the meeting. Ulman hosted a program with other movement science experts teaching best practices on applying motion capture in return to sports decision making. Bioengineer Alex Loewen, M.S., and Ben Johnson, P.A.-C., presented a study on measuring changes in pelvic tilt before and after hip surgery. Ulman and Loewen shared another study designed to improve accuracy of trunk testing across movement science labs. Additionally, biomechanist Ashley Erdman, B.S., M.B.A., presented results of a ballerina survey on pointe readiness.
- Perfectly aligned with her passion, Ulman officially assumed responsibility as chair of the Injury Prevention Research Interest Group and provided her peers with the latest research updates on using movement science to facilitate sports injury prevention protocols.
- Musculoskeletal ultrasound expert and sports medicine physician Jacob C. Jones, M.D., RMSK, gave a report on the state of pediatric musculoskeletal ultrasound to the society attending the conference. His specialty in this methodology solidified him as the top choice to address the group with the latest and greatest in the use of musculoskeletal ultrasound for pediatric sports medicine patients. Additionally, Jones presented a poster addressing the use of diagnostic musculoskeletal ultrasound in gymnasts.
- Shane M. Miller, M.D., concluded his two-year term as chair of the PRiSM Concussion Research Interest Group. This means he led collaborative efforts with others from around the country to improve the identification and treatment of concussions in young athletes and to create a better understanding of the condition. In addition to this national collaboration, our team worked on other concussion projects. Jones shared results of a study on concussions in young athletes, comparing injuries by position in soccer players.
- Elbow and shoulder injuries in throwing athletes continue to be a concern for pediatric sports medicine experts across the country. Sports surgery pair Philip L. Wilson, M.D., and Chuck Wyatt, M.S., CPNP, RNFA, shared results from several projects aimed at improving all aspects of care in two upper extremity scientific sessions. In addition to sharing results of Scottish Rite studies on elbow injuries in young athletes, Wilson shared results from a multi-center group focused on clavicle fractures called FACTS.
- Three of our physical therapists, Jessica Dabis, P.T., D.P.T., O.C.S., Katie Holehouse, P.T., D.P.T., CSCS, and Jacob Landers, P.T., D.P.T., O.C.S., CSCS, presented projects at the meeting.
- Our sports psychologists Emily Stapleton, Psy.D., and Emily Gale, Ph.D., presented on mental health screening tools and the presentation of suicidality in young athletes.
- One of our student interns Sarp Sahin was one of five students awarded a grant from PRiSM to attend and present at the conference. As an undergrad at Washington and Lee University, Sarp was proud to present a novel project that he has been working on since high school. His efforts were recognized by sports medicine clinicians and appreciated by many.
The sports medicine staff’s expertise was shared with other sports medicine clinicians around the country to improve care for young athletes near and far. In return, our team learned valuable information that will impact how we care for young athletes at Scottish Rite. With 23 staff members from the Scottish Rite Sports Medicine team attending, we had a well-rounded, multi-disciplinary representation, and the team returned inspired to continue to contribute to the future of the field of pediatric sports medicine.

Thumb Fracture Q&A
Pediatric nurse practitioner Courtney Schneidau, P.A.-C., shares information about thumb fractures and how to handle these types of injuries in young athletes.
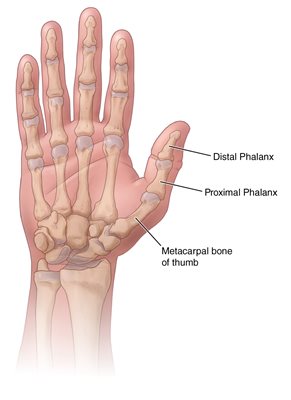
Anatomy of the thumb
The thumb is made up of two major bones — the distal phalanx and the proximal phalanx. The distal phalanx starts at the tip of the thumb, underneath the fingernail and extends to the knuckle. The proximal phalanx runs from the knuckle to the base of the thumb, where it connects to the hand.
How do thumb fractures typically occur?
A thumb fracture can occur anywhere in the thumb and is generally caused by a direct trauma, like from a fall or a hit to the hand. For example, if a player hits his hand/thumb on the helmet of another player while playing football.
What are the main symptoms of a thumb fracture? How do you know if the injury needs medical attention?
Symptoms can include:
– severe pain
– swelling and tenderness
– limited motion or inability to move the thumb
– visible deformity or deformed appearance
– a numb sensation or coldness in the thumb
You should seek medical attention if you are experiencing pain, bruising or swelling. It is important for a professional to examine the injury to determine the best course of treatment.
How is a thumb fracture diagnosed and treated?
Your provider will take a detailed history, including the activity that caused the injury, as well as perform a physical exam. X-rays of the hand and injured thumb will be performed to better evaluate the injury and rule out other injuries.
A fractured thumb can be treated through casting or the use of splints, which limit movement while the bones heal. Surgery is sometimes needed, depending on the location of the break. There are different techniques that are used to hold the bones in place, including the use of pins, plates or screws. Following surgery, a splint or cast is worn to ensure proper healing.
What is the outcome following a thumb fracture?
Thumb fractures generally have good outcomes, following proper treatment and rehabilitation. Once the fracture has healed, hand therapy may be required to help restore motion.
Should you see a pediatric orthopedic specialist for a potential thumb fracture?
Scottish Rite for Children treats children who need complex reconstruction following trauma or have hand disorders related to neurological conditions or nerve injuries. That includes fractures (shoulder to fingers), nerve injuries, tendon injuries and complex injuries. Our Sports Medicine team treats the comprehensive needs of athletes and provides management for sport-related injuries and conditions. Young and growing athletes are highly competitive and have unique conditions that require care by a pediatric team of experts. Learn more about our centers for excellence in Sports Medicine and Hand and how board-certified pediatricians, pediatric orthopedic surgeons, physical therapists, athletic trainers, psychologists and other specialists work side-by-side with each patient and their parents to develop the best game plan for treatment, rehabilitation and safe return to sport.
Learn more about our Facture Clinic.

Fear-Avoidance in Athletes
What is Fear-Avoidance?
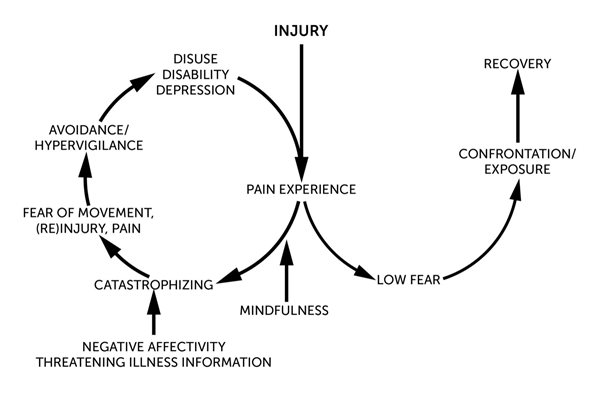
Athletes who experience an injury often struggle with fear-avoidance once they are physically cleared to return to sports. Out of fear of pain or injury, fear-avoidance is when a person develops and maintains chronic pain due to avoiding certain motions or behaviors. “Fear-avoidance is a model that describes how movement and pain-related fear can impact the development and maintenance of chronic pain and increased sensitivity to pain,” pediatric psychologist Emily Stapleton, Psy.D., says. To avoid perceived pain or injury, athletes may believe they cannot complete some rehabilitation exercises and as a result, the athlete may:
- hesitate when completing exercises
- not put in effort
- hold back in training or competition
- increase their dependency on family, coaches or medical team
The more the athlete does these things, the greater the anxiety becomes about pain, movement and reinjury. This fear-avoidance cycle is shown below:
What Does Fear-Avoidance Look Like in the Athlete?
“In athletes, fear-avoidance may look like hesitation when completing necessary exercises for recovery or decreased effort in rehabilitation exercises,” Stapleton says. “You may also see athletes skipping certain physical therapy exercises, discontinuing exercises early, or not completing the number of reps or recommended time due to pain or pain-related fear. Outside of rehabilitation, athletes may avoid social activities or sports where they anticipate the need to engage in increased physical activity, or actions they perceive as unsafe or as likely to increase pain, such as walking long distances or standing for extended periods of time.”
Part of the fear-avoidance cycle includes catastrophizing, or assuming that the worst possible outcome or event will happen. “This pattern of thinking increases distress and is linked to both anxiety and depression,” Stapleton says. In athletes, catastrophizing can manifest in many ways:
- Constant or invasive thoughts about the pain of injury.
- The athlete might think their injury is the worst possible injury and that they will never get back to their pre-injury performance level.
- Believe nothing can be done about their pain or injury, and they will never recover.
This negative thinking can lead to fear of pain, movement, further injury and result in avoidance of anything that might cause pain, make the injury worse or result in another injury. As a result of increased anxiety and avoidance, one can become fixated on monitoring physical sensations in their body and very sensitive toward anything that increases discomfort, even physical therapy exercises that are needed for recovery. This often leads to sedentary behavior and will stop or greatly reduce physical activity levels. “Avoidant behavior is expected and healthy in the immediate acute phase post-injury, as following injury rest is often needed for recovery,” Stapleton says. “However, when returning to activities is appropriate or engagement in physical therapy exercises is necessary to recovery and rehabilitation, avoidance of these activities can actually be harmful, leading to increased pain, chronic pain, and/or declines in mood.”
In athletes, deconditioning often triggers more negative thoughts about their abilities, which can lead to depression and disability. Concerning signs and symptoms of depression include:
- changes in appetite
- changes in sleep
- irritability
- anger
- sadness
- frequent crying or emotional outbursts
- lack of motivation, a decline in academic performance
- disengagement and/or social withdrawal
- substance abuse
It is important to learn strategies to cope with the anxiety so that rehabilitation and recovery are not significantly impacted.
How to Provide Support
There are ways that you can help support your child and work through their range of emotions and fears:
- Help them to identify exercises or activities that increase negative emotions, or triggers. Look for when an athlete becomes distressed, avoids or hesitates prior to certain exercises for clues of triggering activities/exercises.
- Create a hierarchy of the identified triggers and rate them from least to most fearful.
- Start with the least feared exercise and have the athlete perform the task in a controlled and safe environment. Challenge the athlete to increase speed, repetitions and/or difficulty until they are performing without worry.
- Use goal-setting techniques, such as setting SMART goals (specific, measurable, attainable, relevant and timely), to create daily, weekly and monthly goals for building tools to manage anxiety and stress, as well as to do the identified fear exercises.
- Build coping skills to handle fear and worry triggered by pain and movement. Diaphragmatic breathing, positive self-talk and imagery techniques have all been shown to help reduce levels of distress, increase comfort and build confidence during rehabilitation and return to sport.
- Provide education about how fear and decreased confidence can increase their pain and get in the way of their ability to return to their sport.
Learn more and download tips for helping young athletes manage stress.
Psychology Services at Scottish Rite for Children
Our Psychology department has teams of pediatric psychologists at both our Dallas and Frisco campuses. Pediatric psychologists are embedded in the care of each patient, providing support to our sports medicine patients throughout their care and treatment. Learn more about our psychology services.
Emily Stapleton, Psy.D., is a pediatric psychologist at the Frisco campus of Scottish Rite for Children. She specializes in pain management, rehabilitation, coping with acute and chronic illness/injury and sports medicine. She has a particular interest in supporting young athletes following a sport-related injury.

When a Young Athlete Gets Too Hot
As temperatures rise and athletes return to outdoor training and tournaments, recognizing and responding to the signs and symptoms of heat illness is critically important. Though body temperature may not be elevated, heat illness may still be present.
Signs and Symptoms of Heat Illness
- Weakness
- Vomiting
- Excessive thirst
- Headache
- Fatigue
- Sweating
- Nausea
- Light-headedness
Keeping cool when exercising in the heat
- Take rest and water breaks, every 15-20 minutes
- Avoid the hottest hours from 10 a.m. – 5 p.m.
- Drink a sports drink with electrolytes and 6-8 percent carbohydrates when training lasts over 60 minutes
- Avoid training in direct sunlight
- Take breaks in the shade
- Encourage removal of equipment during breaks, e.g., helmet
- Wear loose-fitting, light-colored and moisture-wicking clothing
Be prepared
- Prepare ice and water before training sessions
- Limit consumption of caffeinated and sugary beverages
- Gradually increase physical activity in the heat
- Continue conditioning in the off-season
- Don’t train in the heat while you are sick or have a fever
Ways to respond quickly to signs and symptoms of heat illness
- Full body immersion in an ice bath
- Iced-down towels applied all over the body
Download this infographic with your team and coaches.

.jpg?width=449&height=658)