This is a summary of a program presented as part of a free, monthly education series at Scottish Rite for Children in Frisco, Texas.
Register for this and other on-demand programs or watch the presentation on our YouTube channel for Medical Professionals.
Download a PDF of this summary.
Shane M. Miller, M.D., discussed commonly encountered acute ankle injuries in a young athlete including considerations for safe return to play after an ankle injury.
Ankle injuries are unfortunately very common in young athletes, studies mentioned estimate:
- ankle sprains account for 16% of all injuries.
- ankle injuries represent 22% to 50% of all sport-related injuries presenting to emergency departments.
- one in four of all recurrent injuries among high school athletes are in the ankle.
Additional factors noted about the epidemiology of ankle injuries include:
- Girls have a higher injury rate than boys in soccer, softball/baseball, and track and field, but similar rates are observed in basketball, volleyball and lacrosse.
- Dynamic sports requiring jumping and cutting activities, such as basketball, gymnastics, volleyball, soccer and football account for the majority of acute ankle injuries.
- Indoor court sports and sports that involve player-to-player contact are high risk.
- Sports involving repetitive activities and running, such as cross country, track and field, gymnastics and soccer, are commonly associated with overuse injuries of the ankle.
History and Evaluation
When discussing the athlete’s history, elements to consider include variables beyond age, sex and sport. Knowing the position played, level of competition and history of previous injuries (same side, opposite side, knee, concussion, etc.) will help in understanding the conditions surrounding the injury. Understanding the long-term goals of the athlete and timing (pre-season, playoffs, etc.) helps to customize the treatment planning and anticipate the athlete’s response to the plan.
When assessing the history of the injury, ask:
- Is this the first time you have had any pain or instability in your ankle? (Acute or Chronic?)
- How did the injury occur?
- Was there any swelling?
- Did you hear or feel a pop?
- Were you able to walk on it?
- Were you able to keep playing?
- Can you point with one finger to the location of pain?
- What treatment was provided immediately after it occurred and since that time?
Commonly encountered acute ankle injuries in a young athlete
Using a case-based approach, Miller covered common acute ankle injuries and approaches to evaluation and early management. He reviewed key elements of each case using these questions as a guide:
- What is the most likely diagnosis and mechanism of injury?
- When is imaging necessary and what would you order?
- What does your initial treatment entail?
- When should referral to an orthopedic/sports medicine specialist be made?
Ankle Sprain
A strain is a muscle injury. A sprain is a ligamentous injury, and most, approximately 85%, are inversion injuries and involve the anterior tibial fibular ligament (ATFL) (lateral ankle sprain). Injuries to this and other ligaments are commonly associated with bruising, swelling, inability to bear weight and limited range of motion. These injuries also tend to have a high rate of recurrence or chronic instability.
Imaging
With the presence of bony tenderness, inability to bear weight or significant swelling or bruising, anterior posterior (AP), lateral and mortise views are recommended. Ottawa ankle rules are helpful in determining if X-rays of the ankle are necessary in adults and children. Tenderness in other areas may indicate additional X-rays of the foot. Because an MRI is rarely needed, a specialty referral is indicated if considering an MRI for an ankle sprain. An MRI may be helpful to evaluate for some conditions like occult fractures or more significant injury, such as high ankle sprains or an osteochondral injury.
Treatment
Early treatment of acute injuries of the ankle should include strategies that protect the ankle from further injury, reduce and prevent swelling and promote early mobilization. A familiar pneumonic, “RICE” has been modified to, “PRICEMMS” to include treatment beyond the early acute stage.
- Protection from further injury – walking boot, splint, ankle brace or air stirrup
- Relative Rest – not doing anything that hurts, including the use of crutches if the patient is limping.
- Ice – 20 minutes on the hour may help with pain and to reduce swelling
- Compression – ankle wrap
- Elevation – above the level of the heart
- Medications – analgesics and anti-inflammatories
- Mobilization – improving range of motion using gentle, early mobilization including active dorsiflexion and multi-directional movements, i.e., making letters of the alphabet with the toes.
- Strength – training of the peroneal and gastrocnemius muscles with high repetition, isometric and low resistance exercises, balance exercises and proprioception training
Return to play after an ankle sprain
In general, young athletes with musculoskeletal and cervical spine injuries should not return to play until they have full range of motion, resolution of pain, normal strength, psychological readiness and the ability to demonstrate adequate sport-specific skills.
Return to play criteria should include:
- Absent (or minimal) pain
- Stable ankle with daily activity
- Full range of motion
- Normal strength (>90% of uninjured side)
- Good balance/proprioception
- Able to protect self from further injury
- Functional progression – maneuvers at full speed, no pain
- Restoration of confidence
After considering these items, individual circumstances should be assessed to identify risk of further injury and the need for protective bracing or additional time or treatment prior to returning. In some conditions, a referral to a pediatric sports or orthopedic provider may be advised, these include:
- Confirmed or suspicion for fracture
- Syndesmosis or “high ankle” sprain
- Damage to the anteroinferior tibiofibular ligament (AITFL) and syndesmosis
- Stress in external rotation and dorsiflexion will exacerbate pain.
- May see widening of mortise on X-ray
- Recurrent ankle injuries
- Need for rapid return to sports participation
- Not responding to normal conservative treatment
Physeal Injuries
Physes, commonly referred to as growth plates, are composed primarily of cartilage cells so are more susceptible to both acute and overuse injury. The physis is the “weak link” in the chain and injuries in this area may lead to growth arrest or deformity.
Key terms to know:
- Diaphysis – midshaft, tubular portion of long bone
- Metaphysis – area adjacent to physis, consists of cancellous bone
- Physis – growth plate
- Epiphysis – longitudinal growth center
- Apophysis – growth center that adds contour to a bone
Often a site of muscle/tendon attachment
Ankle Physeal Injuries
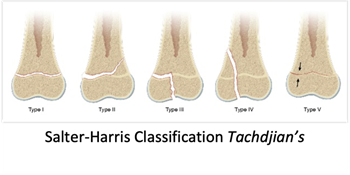
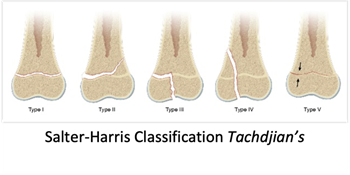
Salter-Harris Fracture Classification
- I and II – don’t involve joint surface, usually do well without surgery
- III, IV and V – involve articular surface, need specialist consultation
- Salter-Harris I – must have high index of suspicion
- X-rays may be negative with Salter-Harris I
- Comparison views may be helpful
- However, they may be less likely than previously thought
- Boot may be preferred over a cast, when immobilization is indicated
- Radiographic stress views are discouraged.
- Beware of the medial ankle sprain—tibial physeal injuries are a more likely diagnosis.
- Occult fractures can cause gait disturbances in young children.
- An ankle injury in a prepubertal adolescent may be a growth plate fracture rather than an ankle sprain.
- Presence of a subfibular ossicle may be related to a prior ankle injury, but treatment is not indicated unless it is symptomatic.
- Transitional fractures include triplane and Tillaux fractures.
- These occur as the growth plate is closing.
- These typically need surgical intervention.
Prevention
Studies reviewed in this presentation compared types of off-the-shelf ankle braces. Results suggest that braces may reduce the incidence but not reduce the severity of ankle, knee or other lower extremity injuries. Balance training was a finding in an article reviewing lateral ankle injury studies. Co-course director and program moderator, Henry B. Ellis, M.D., contributed to this review and provided comments in the Q and A session.
Key Takeaways
- Foot and ankle injuries are very common in young athletes.
- Have a high index of suspicion for fracture and low threshold to obtain X-rays.
- Consider bracing and balance training for prevention of ankle injuries.